Musing 127: Digital Wargames to Enhance Military Medical Evacuation Decision-Making
Very interesting piece out of Berkeley, Stanford and the US Army
Today’s paper: Digital Wargames to Enhance Military Medical Evacuation Decision-Making. July 10, 2025. Fischer et al. https://arxiv.org/pdf/2507.06373
Not many people draw a connection between war and games at first blush, but the connection between the two has always been deep and meaningful. Carl Von Clausewitz, regarded as one of the greatest war theorists, was among the first more than a hundred years ago to acknowledge the strong collaborative relationship between war and games. While the use of wargames in training dates back centuries, during the 1970s and 1980s, the United States Defense Science Board recognized wargames as a “revolution in training”, drastically improving unit proficiency within a short timeframe. DARPA’s DARWARS program demonstrated how these simulations/games could provide realistic decision-making experiences for military personnel. Perla’s The Art of Wargaming emphasizes the value of decision-making in professional military wargames, suggesting that effective play requires participants to understand real-world problems and apply strategic thinking.
It can be a mistake (albeit, an understandable one) though to think that wargames is all about war, as we understand the term. It is true that modern combat preparedness increasingly relies on digital wargames and simulation software to enhance operational decision-making and crisis response. For example, the Combat Simulation Lab at West Point employs advanced tools like IWARS, JCATS, OneSAF, and VBS2, designed for tactical engagement modeling, infantry warfare simulations, semi-automated battlefield scenarios, and immersive first-person training. These systems enhance decision-making and operational readiness by providing realistic environments for cadets and faculty to test and refine operational strategies.
Despite their advanced proficiencies and ability to replicate friction and uncertainty on the battlefield, these games do not contain a medical evacuation component. That’s what today’s paper is all about. Non-military medical and emergency response training simulators continue to advance significantly. Medical education has incorporated simulation-based methodologies, ranging from mannequin-based training to complex virtual environments in software like Unity. Various simulation-based trainings have been shown to enhance crisis management skills, particularly in emergency medical scenarios. For example, emergency care digital simulations have successfully replicated first-aid training while reflecting the stress and chaos of the environment. Furthermore, Unmanned Aircraft Systems (UAS) are being controlled by players in a manufactured environment to simulate opioid overdoses in rural areas, demonstrating the benefit of these games in emergency response education.
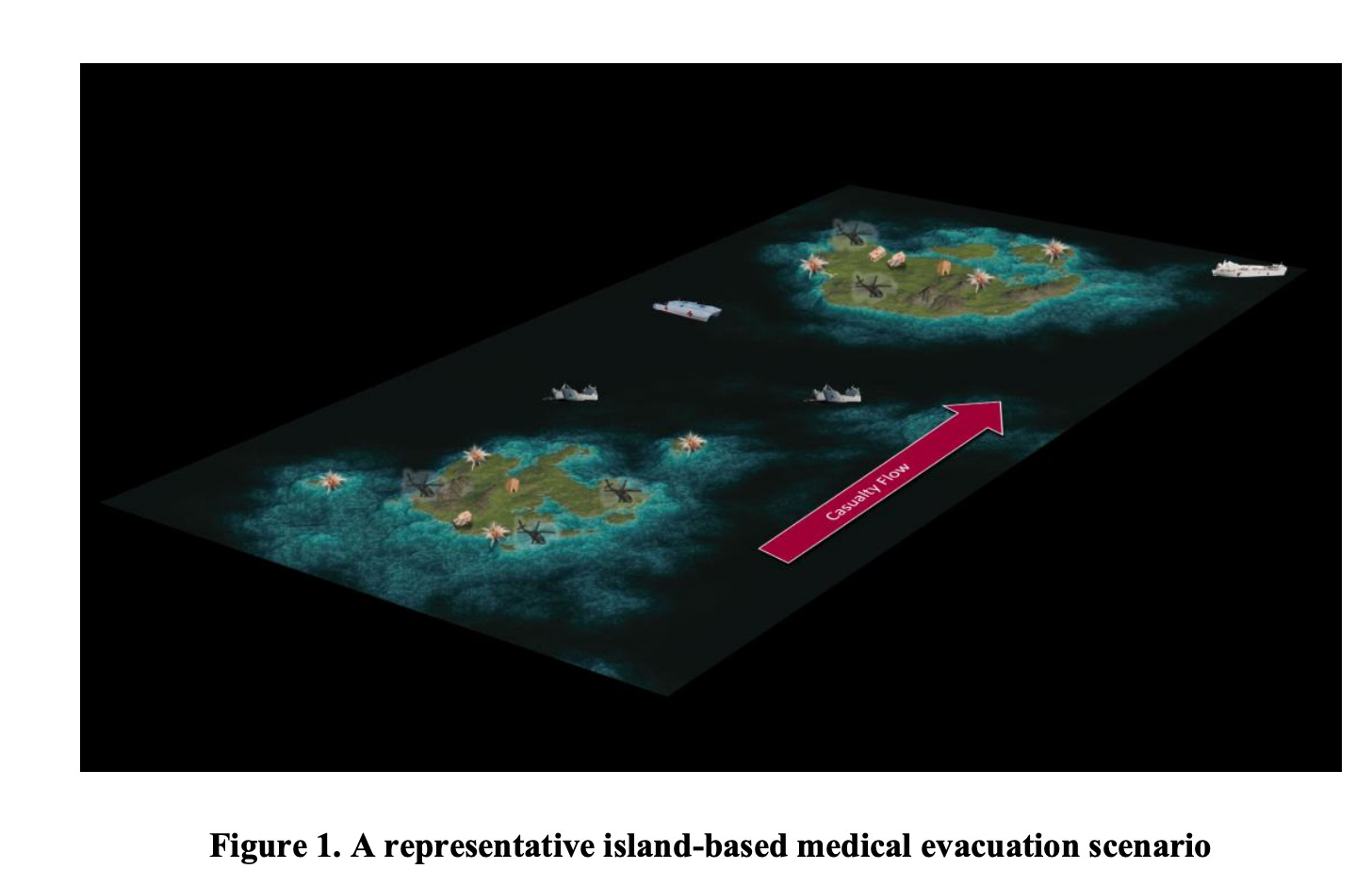
What are the objectives of a ‘medical wargame’? The paper dives headfirst into the Medical Evacuation Wargaming Initiative (MEWI) that was developed for the United States Army’s Medical Evacuation Doctrine Course at the Department of Aviation Medicine in partnership with the University of California Berkeley’s Mechanical Engineering Department. Medical evacuation planning for complex operational environments, as shown in Figure 1 below, is challenged by limited and diverse evacuation resources, substantial and evolving casualty movement requirements, enemy threat considerations, partial system observability, expansive terrain, joint service integration, and other constraints.
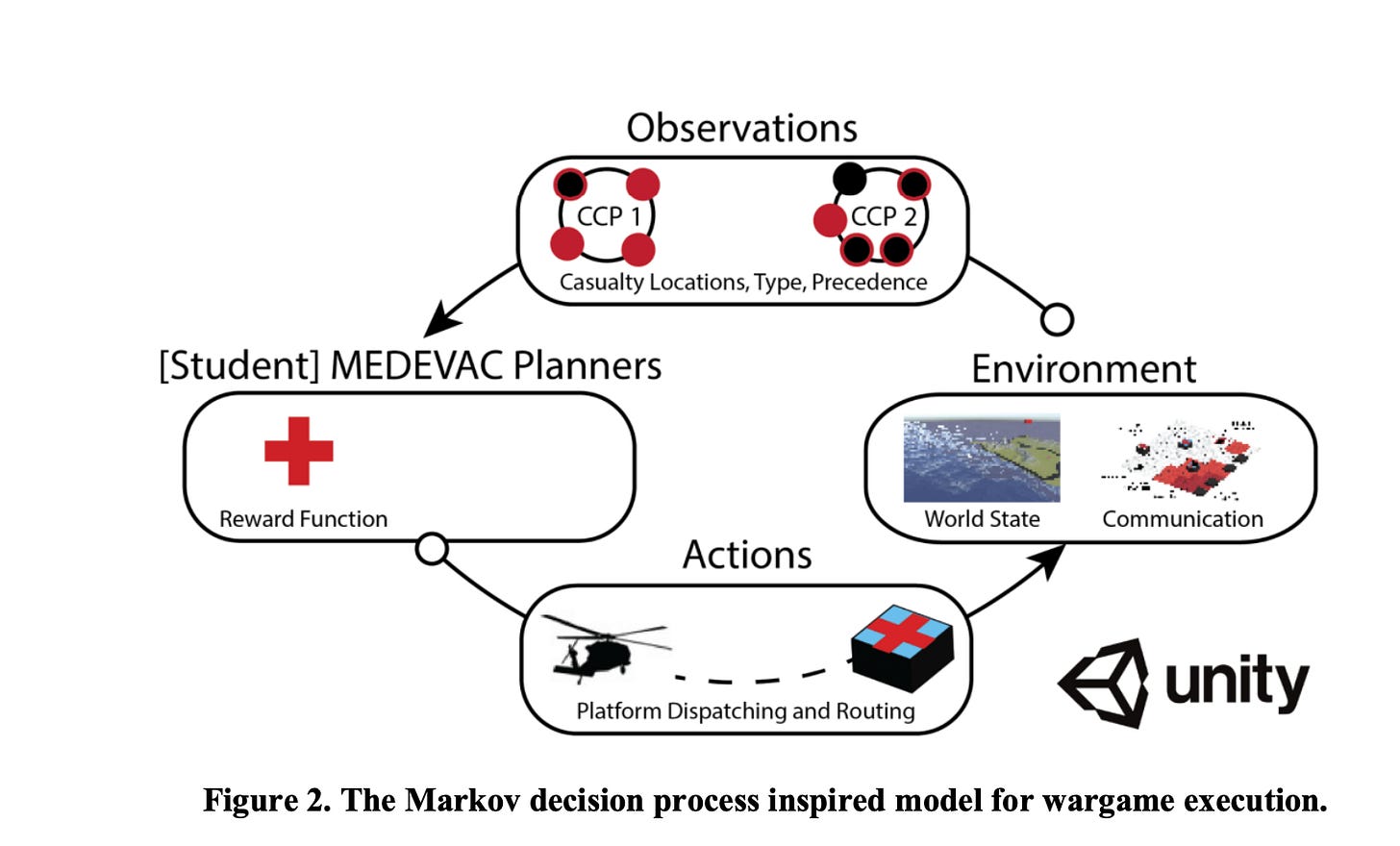
MEWI is the first high-fidelity three-dimensional digital simulation tool dedicated to improving military medical evacuation decision-making in a classroom setting. Examples of evacuation decisions made in the wargames include: how to move patients from various collection points to increasingly sophisticated medical treatment facilities, which platforms will facilitate various legs of this movement, how to triage patients throughout the evacuation process, how to balance limited bed space across the battlefield and minimize transport delays, and how to document patient information and status in space and time. The authors loosely model the interactive MEWI environment, shown in Figure 2 below, on a multi-agent, sometimes partially observable, and often semi-Markovian variant of the Markov Decision Process (MDP). The MDP is a foundational model in the artificial intelligence subfields of planning and learning. At a minimum, it includes states, a state transition function, agents, their actions, and a reward function.
Key components of the MDP are described below:
Agents: Each player in the simulation controls one or more evacuation assets—such as helicopters, ships, or ground vehicles—operating under a shared objective. These players, or “agents,” must make real-time decisions within a dynamic environment, where one agent’s actions can directly impact another’s. For instance, if two helicopters try to land on the same one-pad ship, the second one must wait (introducing a layer of coordination complexity and resource contention).
Reward function: The game rewards players for evacuating patients as quickly as possible, effectively simulating life-saving outcomes. Each patient tracks timestamps across different stages of care: from initial triage (T0), to arrival at frontline care (Role 1, T1), intermediate facilities (Role 2, T2), and finally, to full-service field hospitals (Role 3, T3). These roles escalate in medical capability, with Role 1 handling trauma stabilization and Role 3 providing surgical care and mass-capacity treatment. The faster patients move through this chain, the higher the player’s reward.
Actions: Agent actions reflect realistic medical evacuation decision-making and include:
Aligning specific evacuation platforms to specific evacuation requests
The movement of evacuation platforms around the map
Picking up or dropping off casualties at Role 1, 2 or 3 medical treatment facilities
Organizing patient transfers at exchange locations to include Ambulance Exchange Points (AXPs) and Helicopter Landing Zones (HLZs)
Waiting, as patients cannot be left alone at exchange locations, and transfer times may require platform loitering.
States: The wargame state space includes information relevant to player decision-making at any given time step. Some state information is provided to students prior to wargame execution through scenario-specific planning products and briefings. Most state information should be considered in real-time during gameplay. Agents know their platform locations and capacities, as well as key casualty information including patient precedence (urgent or priority), patient type (litter or ambulatory), and current location. Other known elements include all exchange points, other agent platforms, and threat zones.
Transitions: State transitions within MEWI are driven by a mix of stochastic and deterministic processes in response to agent and adversarial actions. The adversarial agent places threat rings over transit routes, causing arrival times and planned routes to shift. Casualty generation at collection points follows a Poisson distribution, introducing randomness to when and how many patients are produced.
Observations: State information may be intentionally hidden from players, whether due to fog of war constraints or the nighttime cycle. This forces players to plan using incomplete or noisy observations of the state space, which can result in suboptimal decision-making. Partial observability encourages players to communicate their observations with one another outside of the confines of the digital wargame. Agent coordination is critical to success, as how well players communicate outside of the wargame heavily influences what parts of the overall state they can effectively observe and act on.
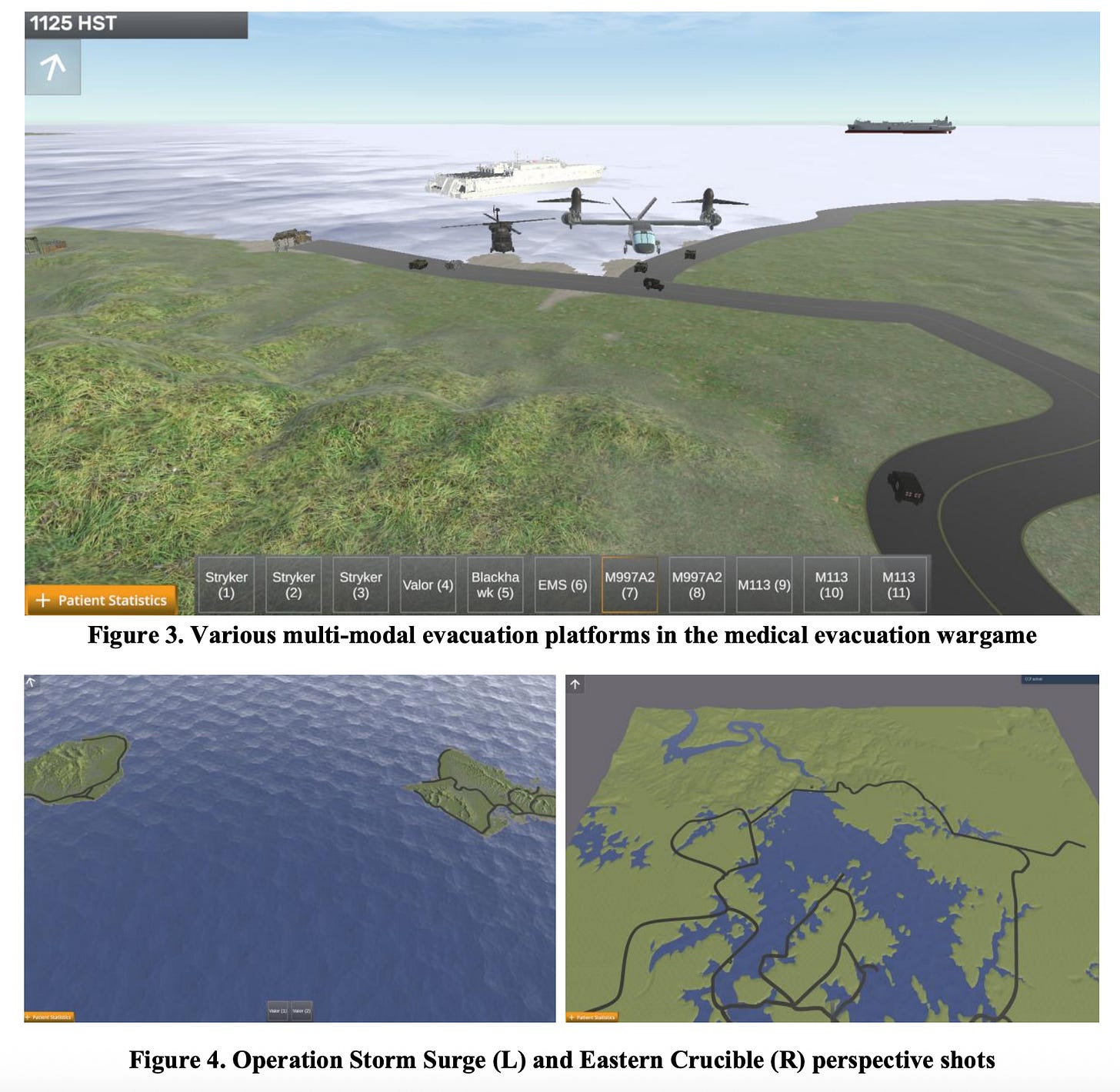
The game contains two scenarios: Operation Storm Surge and Operation Eastern Crucible (Figure 4). The former is set in the Hawaiian Islands and centers on an amphibious assault involving mass casualty events. Participants must manage patient evacuations from multiple casualty collection points (CCPs) across two islands using a mix of helicopters, ships, and ground vehicles to reach offshore hospital ships. The scenario reflects the U.S. military’s renewed focus on littoral and amphibious operations. Operation Eastern Crucible, takes place in Eastern Europe and emphasizes land-based operations across complex terrain and critical road networks. As CCPs activate and deactivate with shifting front lines, participants must continuously adapt their evacuation strategies using both ground and air assets to ensure timely medical care.
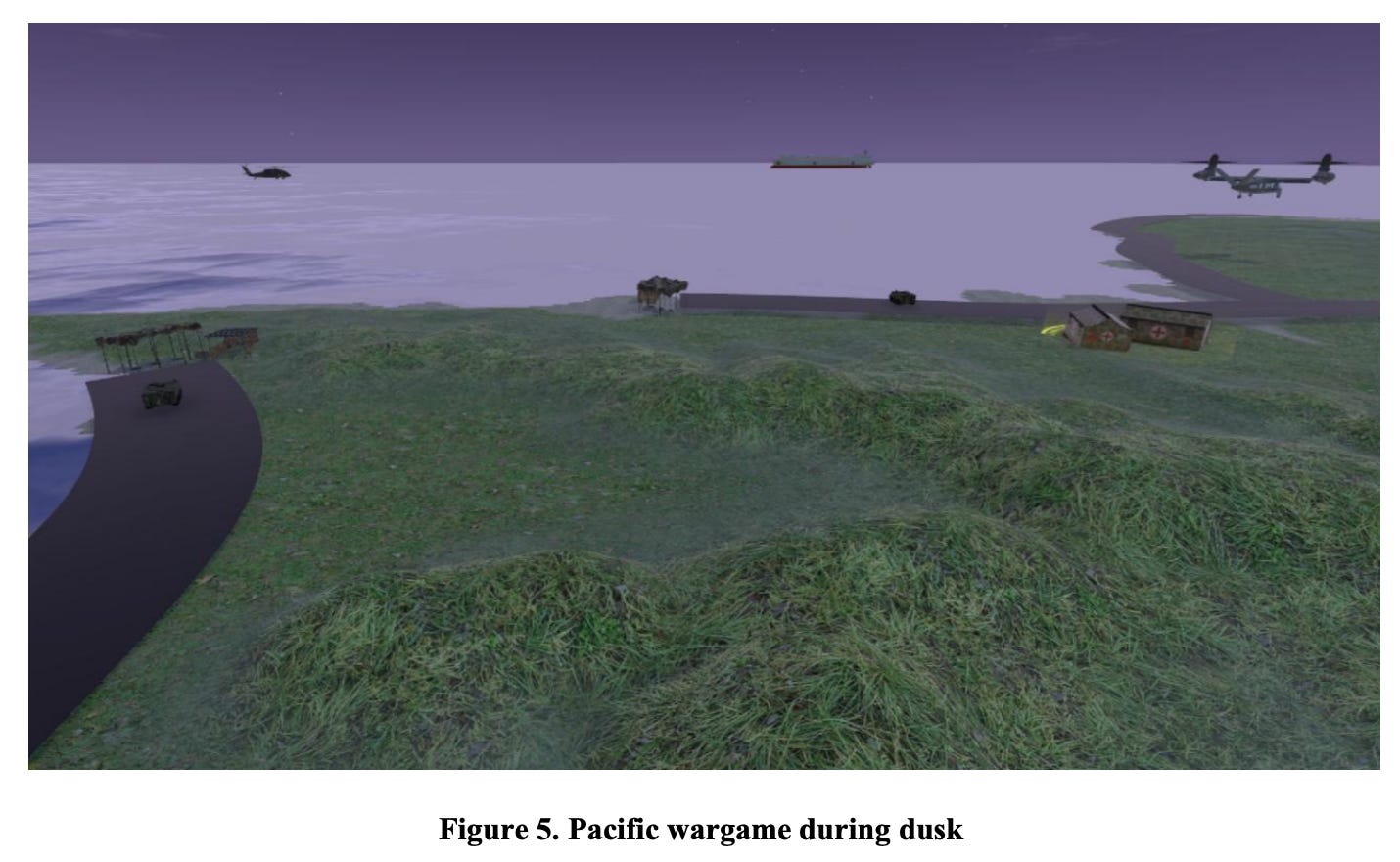
To inject realism into the simulation, the wargame designers introduced three core features: limited information, policy constraints, and instructor injects. Under the limited information category, participants operate under conditions akin to the real-world "fog of war." They begin with only generalized knowledge of the battlefield, and once gameplay starts, they contend with dynamic day-night cycles (Figure 5 below) that affect visibility, adversarial threat zones generated by AI agents (Figure 6 below), stochastic casualty surges, and limited knowledge of patient status beyond urgency. Together, these variables force players to adapt continuously and communicate effectively, as no single participant has a complete view of the scenario.
The policy constraints layer ensures fidelity to real-world Army doctrine. These include strict rules like the one-hour evacuation standard for urgent patients, platform-specific capacity limitations (e.g., litter vs. ambulatory patients), and mandatory adherence to the Role 1 → Role 2 → Role 3 medical pathway without skipping levels. Even practical nuances, like aircraft queuing at single-landing hospital ships and accurate time-distance scaling using real-world terrain maps, are modeled.
Lastly, instructor injects provide an additional axis of unpredictability. Instructors can simulate mass casualty events, selectively activate or deactivate casualty collection points, or impose communication blackouts mid-game to stress-test student coordination. Instructors also have the ability to dispatch non-dedicated evacuation platforms—vehicles without medical equipment or red cross markings—to test how well students integrate improvised resources under pressure. This triad of realism, rules, and reactive instruction transforms the wargame into an immersive, high-stakes learning environment for tactical medical decision-making.
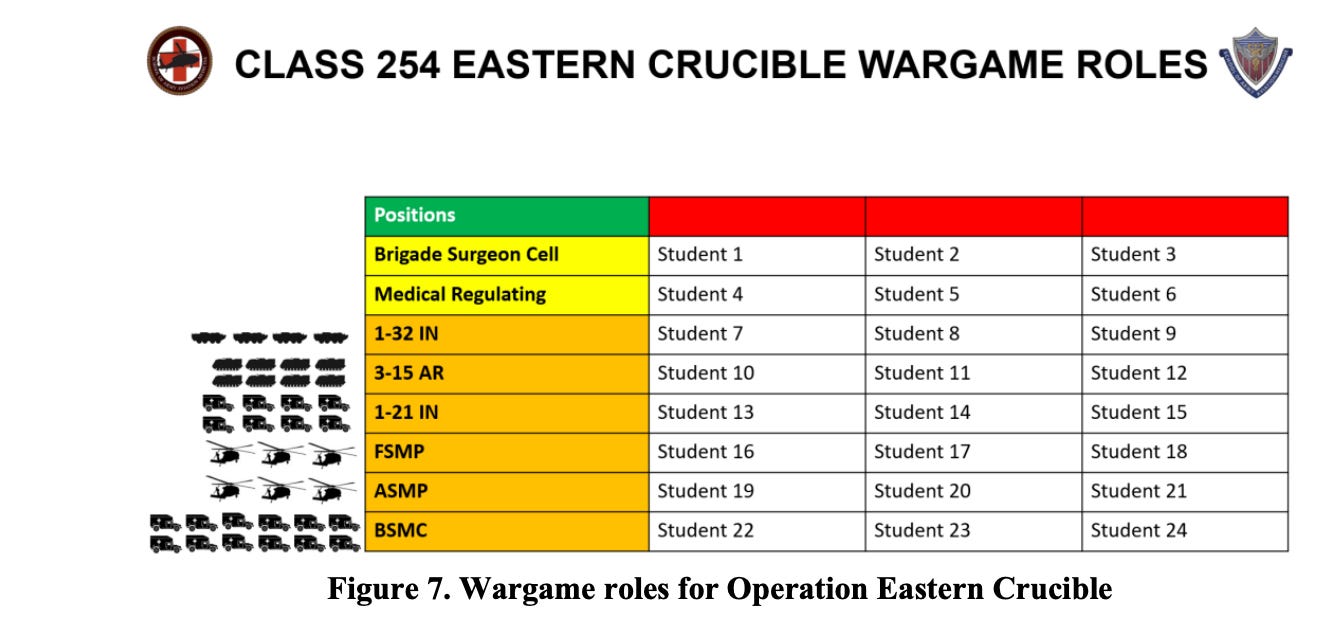
How well does this work? As shown in Figure 7 below, each student is assigned a position associated with the tactical medical evacuation plan for a given scenario.
Positions in orange possess evacuation platforms that need to be allocated and dispatched in the wargame, while positions in yellow are primarily concerned with command and control, and information management. Each position is discussed during the instructor-driven wargame tutorial and during the road to war briefing. The types of medical evacuation decisions to be made in planning differ by position, although the positions are interdependent. 1-32 IN, 3-15 AR, and 1-21 IN are examples of ground maneuver battalions, the forward support medical evacuation platoon (FSMP) and area support medical evacuation platoon (ASMP) are responsible for aeromedical evacuation support, and the brigade support medical company (BSMC) is effectively the Role 2 medical treatment facility. Medical regulators must collect location and medical condition information on all patients transiting the evacuation system in realtime. The brigade surgeon is the overall medical authority for the wargame and is responsible for ensuring the evacuation system runs smoothly. In larger groups, participants may be separated into two distinct teams competing against each other.
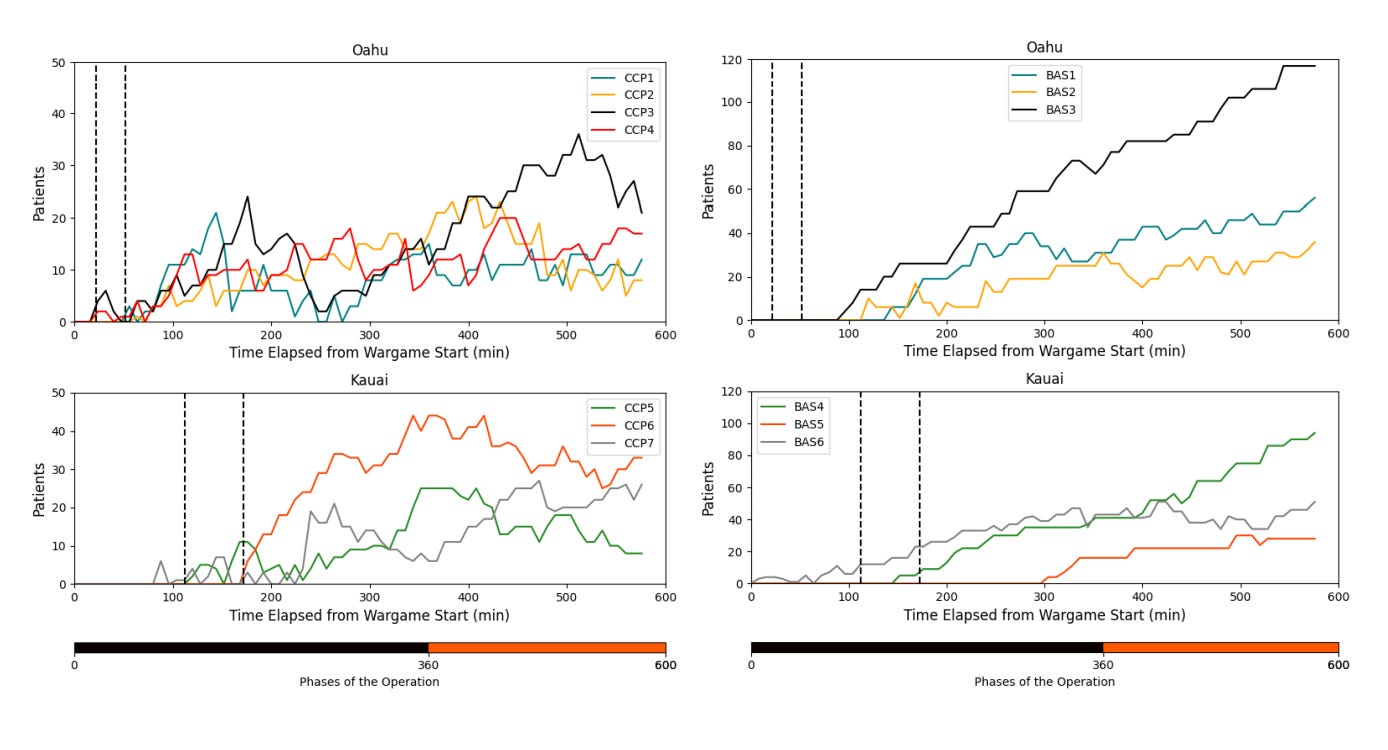
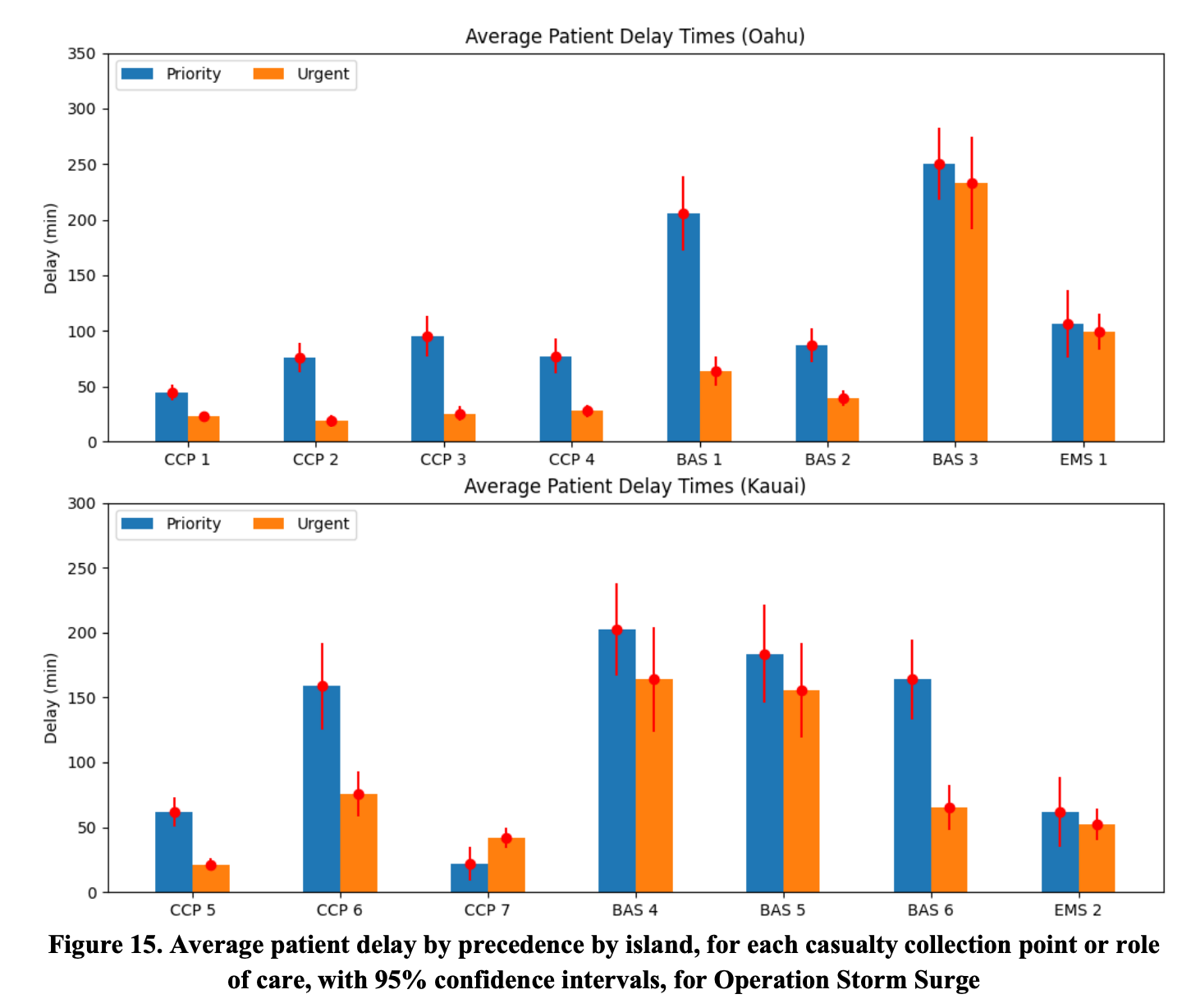
In analyzing the results from Operation Storm Surge, several instructive patterns emerged. Students generally succeeded in prioritizing urgent patients over priority ones, adhering to doctrinal expectations and the game’s scoring incentives. However, even with effective triage, most urgent patients failed to meet the one-hour evacuation standard to Role 2 facilities—mirroring a widely acknowledged real-world concern in large-scale combat operations. Students on Oahu performed better at maintaining this prioritization across casualty collection points (CCPs), but performance faltered at the Role 1 level, where delays accumulated. On Kauai, remote CCPs like CCP 6 were underserved, partly due to limited platform reallocation and poor anticipation of geography-based logistical bottlenecks.
Another key lesson was the tendency to over-rely on air platforms—particularly the high-speed V-280 Valor helicopters—while underutilizing ground vehicles. This imbalance reflects a broader operational challenge in military planning: the assumption that air evacuation will always be available and sufficient. Ground routes, though slower, are essential for coverage, especially when air assets are delayed or overwhelmed. Students also learned that continuity of care—ensuring that patients move sequentially through Roles 1 to 3—can unintentionally create chokepoints if upstream facilities are not cleared quickly. Perhaps most importantly, the wargame emphasized the importance of forward-thinking asset placement and cross-team coordination, especially in responding to unexpected events like the instructor-triggered MASCAL (mass casualty) scenario. Both teams struggled to adapt quickly, underscoring the critical need for dynamic planning in medical evacuation operations.
As a specific example, Figure 15 presents average patient delay by precedence, stratified by island and across CCPs and roles of care. A delay is defined as the time a patient spends at a medical facility after having received treatment but before being picked up by an evacuation platform, or for CCPs, the time a patient spends after initializing but prior to initial pick up by an evacuation platform. Delay times for urgent patients at all Oahu CCPs and BAS 1 and BAS 2 were significantly less than delay times for priority patients; this indicates that wargame participants on Oahu performed adequate triage at those locations. Oahu wargame participants failed to meaningfully triage at BAS 3 or from the Oahu-affiliated Role 2 expeditionary medical ship. Similarly, wargame participants on Kauai performed adequate triage at CCP 5, CCP 6, and BAS 6, but failed to do so at CCP 7, BAS 4, BAS 5, or the Kauai-affiliated Role 2 expeditionary medical ship.
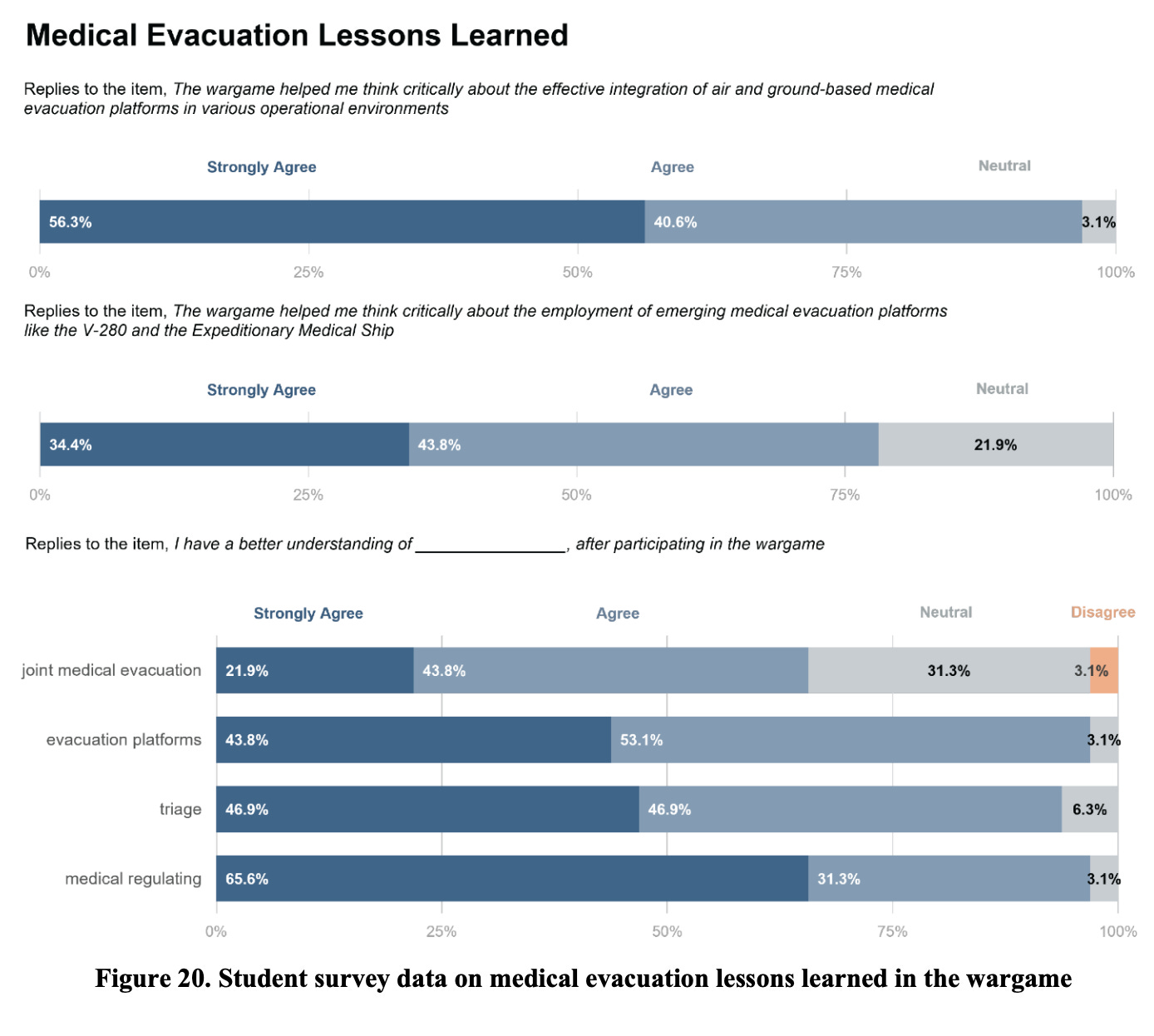
In closing the musing, I thought this was a very interesting paper that covers some important points, contains real data and lots of great visuals. Students really believed that they had a much better understanding of medical evacuations and related aspects following the wargaming:
However, there are some limitations. One limitation of this research study is the need for repeatability to assess learning retention and improvement. Due to the intensive and fast-paced nature of military schoolhouses, students participated in each wargame scenario only once. While the Likert surveys measured learning, students did not have the opportunity to replay the same scenarios and apply lessons learned in quick succession. This limits the assessment of skill progression within the wargame. Also, the wargame lacks a few critical features, currently in development, that affect medical evacuation decision-making. Fuel and fighter management considerations limit the employment of evacuation platforms to specific ranges and time windows and can induce substantial delays if not appropriately planned. A significant forthcoming development is the implementation of an adversarial intelligent agent that generates enemy threat rings and selects which CCPs patients should be initialized at. The adversarial intelligent agent, trained using the Proximal Policy Optimization algorithm, remains in testing. Once fully integrated, having an intelligent enemy will provide valuable insights into evacuation planning around threats, increase wargame difficulty, emphasize the need for participant communication, and add realism.